Market Manager Utilization Review
The posted compensation range of $51.66 - $74.91 /hour is a reasonable estimate that extends from the lowest to the highest pay CommonSpirit in good faith believes it might pay for this particular job, based on the circumstances at the time of posting. CommonSpirit may ultimately pay more or less than the posted range as permitted by law.
Located conveniently in the heart of Phoenix, Arizona,St. Joseph's Hospital and Medical Center is a 571-bed, not-for-profit hospital that provides a wide range of health, social and support services. Founded in 1895 by the Sisters of Mercy, St. Joseph's was the first hospital in the Phoenix area. More than 125 years later, St. Joseph's remains dedicated to its mission of caring for the poor and underserved.
We are extremely proud to be a nationally recognized center for quality quaternary care, medical education and research. St. Joseph's includes the internationally renowned Barrow Neurological Institute, Norton Thoracic Institute, Cancer Center at St. Joseph's, Ivy Brain Tumor Center, and St. Joseph's Level I Trauma Center (which is verified by the American College of Surgeons). The hospital is also a respected center for high-risk obstetrics, neuro-rehabilitation, orthopedics, and other medical services. St. Joseph’s is considered a sought-after destination hospital for treating the most complex cases from throughout the world. Every day, approximately 20 percent of the hospital’s patients have traveled from outside of Arizona and the United States to seek treatment at St. Joseph’s.
U.S News & World Report routinely ranks St. Joseph's among the top hospitals in the United States for neurology and neurosurgery. In addition, St. Joseph's boasts the Creighton University School of Medicine at St. Joseph's, and a strategic alliance with Phoenix Children's Hospital.
St. Joseph's is consistently named an outstanding place to work and one of Arizona's healthiest employers. Come grow your career with one of Arizona's Most Admired Companies.
Look for us on Facebookand follow us on Twitter.
For the health of our community ... we are proud to be a tobacco-free campus.
Responsibilities
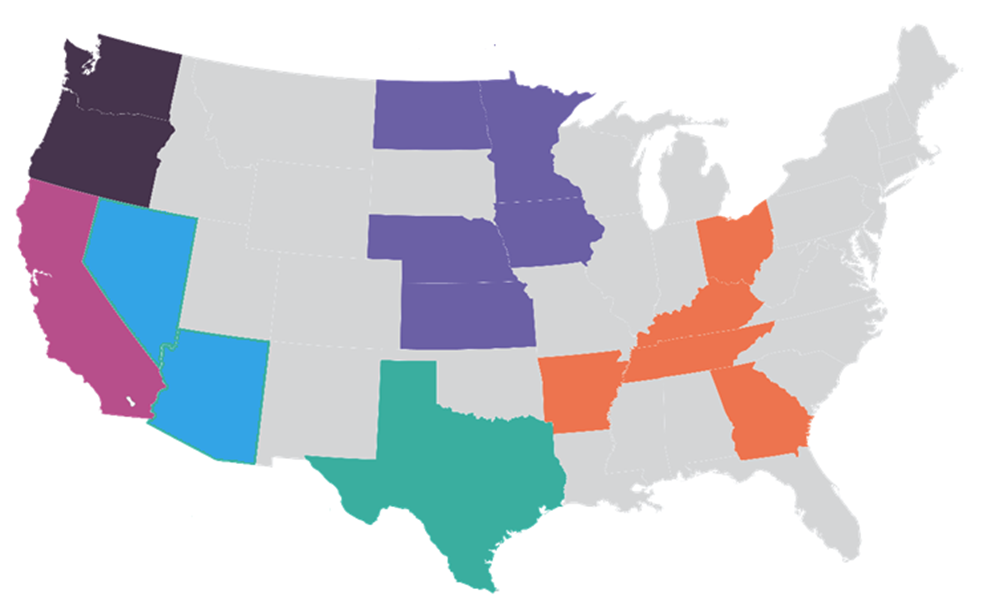
This role is for the Arizona and Nevada markets. Must have current Arizona unrestricted RN license.
The Utilization Management (UM) Manager is responsible for managing day-to-day UM operations within the markets, focusing on
effective team management, authorizations, inpatient admission and continued stay reviews, retrospective authorizations utilizing
standardized criteria to determine medical necessity; reviews and processes concurrent denials that require medical necessity
determinations; processes appeals and reconsiderations. Act as a working manager within Utilization Management, performing
essential duties and responsibilities (utilization reviews, denials, and authorizations) in non-represented markets, with a time
allocation of no more than 40% of the total work hours. Ensure a balance between management and operational responsibilities to maintain effective team leadership and oversight. This role supports the UM Director in ensuring efficient operations with all
processes, policies, strategies and ensuring compliance with all regulatory and payer requirements.
Responsibilities:
- Assist with daily operations of care coordination, including effective staff supervision, and resource allocation to align with
organizational goals. - Oversee staff recruitment, performance evaluation, coaching, mentoring, and professional development, ensuring a
high-performing team aligned with organizational objectives. - Oversee daily operations to ensure effective utilization reviews, strict adherence to denial management processes, and
compliance with established policies and procedures. - Ensure prompt and accurate processing of payer communications and authorizations through efficient management by the UM
staff. - Train and mentor UM staff to promote high performance and adherence to regulatory and organizational standards.
Dignity Health now offers an Education Benefit program for benefit-eligible employees after 180 days. This program provides debt relief and student loan assistance to help you achieve your goals. Full-time employees can receive up to $18,000 over five years, while part-time employees can receive up to $9,000.
Qualifications
Minimum:
- Bachelor's degree in Nursing, Health Care Administration or related clinical field
- Minimum 5 years of clinical case management (Utilization Management, Denial Management, Care Coordination)
- Minimum 3 years management experience in a clinical case management department.(Utilization Management,Denial Management,Care Coordination)
- Current unrestricted Arizona and Nevada RN license
- National certification of any of the following: CCM (Certified Case Manager), ACM (Accredited Case Manager) required or within 2 years upon hire.
Qualified candidates will have the following knowledge and skills:
- Comprehensive knowledge of utilization management
- Medicare, Medicaid, and commercial admission and review requirements
- In-depth knowledge of utilization management processes and best practices
- Strong managerial and decision-making skills
- Excellent communication skills and the ability to work collaboratively.
- Proficient in healthcare IT systems relevant to utilization management
- Effective leadership and team-building skills
- Excellent organizational and communication skills
- Ability to work unde rpressure and manage multiple priorities
- Knowledge of CMS standards and requirements
- Ability to work as a team player and assist other members of the team where needed.
We prefer candidates with:
- Master's degree in Nursing,Health Care Administration or related clinical field.
- Experience with DRG, reimbursement, pricing and coding processes for inpatient and outpatient services
Unless directed by a Collective Bargaining Agreement, applications for this position will be considered on a rolling basis. CommonSpirit Health cannot anticipate the date by which a successful candidate may be identified.
Apply
Depending on the position offered, CommonSpirit Health offers a generous benefit package, including but not limited to medical, prescription drug, dental, vision plans, life insurance, paid time off (full-time benefit eligible employees may receive a minimum of 14 paid time off days, including holidays annually), tuition reimbursement, retirement plan benefit(s) including, but not limited to, 401(k), 403(b), and other defined benefits offerings, as may be amended from time to time. For more information, please visit https://www.commonspirit.careers/benefits.
No featured jobs
No recently viewed jobs
You have no saved jobs
-
 Our Mission and Vision CommonSpirit was created by the alignment of health care organizations to serve as a single ministry of change.
Our Mission and Vision CommonSpirit was created by the alignment of health care organizations to serve as a single ministry of change. -
 Diversity & Inclusion At CommonSpirit, we are dedicated to delivering humankindness. Diversity is not just an initiative, it’s the true nature of who we are. Related Content
Diversity & Inclusion At CommonSpirit, we are dedicated to delivering humankindness. Diversity is not just an initiative, it’s the true nature of who we are. Related Content -
 Nursing Explore more about nursing opportunities, our nursing vision and hear from our staff members. Related Content
Nursing Explore more about nursing opportunities, our nursing vision and hear from our staff members. Related Content -
 Our Benefits Our benefits and perks are a big part of why we’re ranked a top employer. Related Content
Our Benefits Our benefits and perks are a big part of why we’re ranked a top employer. Related Content -
 Saved Jobs Saved Jobs
Saved Jobs Saved Jobs -
 Legal and Privacy Notices Legal and Privacy Notices
Legal and Privacy Notices Legal and Privacy Notices -
 Terms of Service Terms of Service
Terms of Service Terms of Service -
 Website Privacy Notice Website Privacy Notice
Website Privacy Notice Website Privacy Notice -
 Online Accessibility Notice Online Accessibility Notice
Online Accessibility Notice Online Accessibility Notice -
 Copyrights Copyrights
Copyrights Copyrights -
 Application Notices and Information Learn about CommonSpirit Health's application process, important notices, and requirements. Hiring Process
Application Notices and Information Learn about CommonSpirit Health's application process, important notices, and requirements. Hiring Process -
 CommonSpirit Health Alumni Community Interested in returning to CommonSpirit Health? Learn about jobs, company news, and hear from our employees. Hiring Process Blog
CommonSpirit Health Alumni Community Interested in returning to CommonSpirit Health? Learn about jobs, company news, and hear from our employees. Hiring Process Blog -
 Operations Track .The CommonSpirit Health Administrative Fellowship Operations Track will provide fellows with a broad range of health care experiences at the national and local level.
Operations Track .The CommonSpirit Health Administrative Fellowship Operations Track will provide fellows with a broad range of health care experiences at the national and local level. -
 Mission Track The CommonSpirit Health Administrative Fellowship Mission Track Fellow will work directly with mission leadership to develop leadership competencies in Mission Integration, Spiritual Care, Community Health, Ethics, and Ministry Formation.
Mission Track The CommonSpirit Health Administrative Fellowship Mission Track Fellow will work directly with mission leadership to develop leadership competencies in Mission Integration, Spiritual Care, Community Health, Ethics, and Ministry Formation. -
 COVID-19 Vaccination Requirements COVID-19 Vaccination Requirements at CommonSpirit Health
COVID-19 Vaccination Requirements COVID-19 Vaccination Requirements at CommonSpirit Health -
 Clinical Engineering Careers at CommonSpirit Health A career in clinical engineering offers a fulfilling blend of technology and healthcare, with the potential to make a positive impact on patient outcomes and the overall efficiency of healthcare delivery. Learn more and explore a career in clinical engineering at CommonSpirit Health. Hiring Process Blog
Clinical Engineering Careers at CommonSpirit Health A career in clinical engineering offers a fulfilling blend of technology and healthcare, with the potential to make a positive impact on patient outcomes and the overall efficiency of healthcare delivery. Learn more and explore a career in clinical engineering at CommonSpirit Health. Hiring Process Blog -
 Learn about our National Travel Nurse Program Join our National Travel Nursing Program and enjoy the variety of a travel nurse with the security of being employed by one of the largest faith-based healthcare systems in the country.
Learn about our National Travel Nurse Program Join our National Travel Nursing Program and enjoy the variety of a travel nurse with the security of being employed by one of the largest faith-based healthcare systems in the country. -
 Learn about our Virtually Integrated Nursing Care Model Virtually Integrated Care provides assistance to the bedside team and patient/family through the use of virtual technology
Learn about our Virtually Integrated Nursing Care Model Virtually Integrated Care provides assistance to the bedside team and patient/family through the use of virtual technology -
 Military At CommonSpirit Health, we deeply value the sacrifices made by our veterans and their families. Our commitment to supporting those who served extends beyond words—reflected in the opportunities and benefits we provide. Related Content
Military At CommonSpirit Health, we deeply value the sacrifices made by our veterans and their families. Our commitment to supporting those who served extends beyond words—reflected in the opportunities and benefits we provide. Related Content -
 VMFH Hiring our Heroes VMFH HIring our Heroes
VMFH Hiring our Heroes VMFH HIring our Heroes -
 CHI Health 2025 Nursing Internship CHI Health Nursing Internship in Nebraska Hiring Process Blog
CHI Health 2025 Nursing Internship CHI Health Nursing Internship in Nebraska Hiring Process Blog -
 Upper Midwest Now is the perfect time to join our healthcare team in one of our Upper Midwest locations in Minnesota and North Dakota! Hiring Process Blog
Upper Midwest Now is the perfect time to join our healthcare team in one of our Upper Midwest locations in Minnesota and North Dakota! Hiring Process Blog -
 New Grad Nurse Residency and Transition Program for RNs in California Learn about New Grad Residency and Transition or Fellowship Program for RNs in California Hiring Process Blog
New Grad Nurse Residency and Transition Program for RNs in California Learn about New Grad Residency and Transition or Fellowship Program for RNs in California Hiring Process Blog -
 DHMF benefits at a glance 2024 non represented DHMF benefits at a glance 2024 (non-represented)
DHMF benefits at a glance 2024 non represented DHMF benefits at a glance 2024 (non-represented) -
 DHMSO benefits at a glance 2024 DHMSO benefits at a glance 2024
DHMSO benefits at a glance 2024 DHMSO benefits at a glance 2024 -
 DHMF CNA Represented benefits 2024 DHMF CNA Represented benefits 2024
DHMF CNA Represented benefits 2024 DHMF CNA Represented benefits 2024 -
 DHMF Woodland Benefits 2024 Non Represented DHMF Woodland Benefits 2024 Non Represented
DHMF Woodland Benefits 2024 Non Represented DHMF Woodland Benefits 2024 Non Represented -
 DHMF Benefits Summary 2024 SEIU Represented DHMF Benefits Summary 2024 SEIU Represented
DHMF Benefits Summary 2024 SEIU Represented DHMF Benefits Summary 2024 SEIU Represented -
 SoCal Benefits at a Glance 2024 SoCal Benefits at a Glance 2024
SoCal Benefits at a Glance 2024 SoCal Benefits at a Glance 2024 -
 Innovative Virtual Nursing Model CommonSpirit has two types of virtual nurses: ones who work at a command center to help with admissions, discharges and transfers, and ones who are part of the care team, attending rounds with physicians and being available to patients at the push of the button. Hiring Process Blog
Innovative Virtual Nursing Model CommonSpirit has two types of virtual nurses: ones who work at a command center to help with admissions, discharges and transfers, and ones who are part of the care team, attending rounds with physicians and being available to patients at the push of the button. Hiring Process Blog -
 Radiology Careers at CommonSpirit Health Discover fulfilling career opportunities in Imaging Services at CommonSpirit Health and play a vital role in the diagnosis and treatment of patients' care plans. Hiring Process Blog
Radiology Careers at CommonSpirit Health Discover fulfilling career opportunities in Imaging Services at CommonSpirit Health and play a vital role in the diagnosis and treatment of patients' care plans. Hiring Process Blog -
 Elevate your career as a Surgical Tech with CommonSpirit Health As a surgical technician at CommonSpirit Health, you will play a vital role in guaranteeing that surgical procedures are safe and successful. You will collaborate with leading surgeons and healthcare experts in cutting-edge facilities, providing our patients with the utmost care. Hiring Process Blog
Elevate your career as a Surgical Tech with CommonSpirit Health As a surgical technician at CommonSpirit Health, you will play a vital role in guaranteeing that surgical procedures are safe and successful. You will collaborate with leading surgeons and healthcare experts in cutting-edge facilities, providing our patients with the utmost care. Hiring Process Blog -
 Virtual Command Center Ever wondered what it was like to work in a Virtual Command Center? We’re in the background continuously assessing, reviewing and providing interventions to patients at all hours of the day across the nation. Hiring Process
Virtual Command Center Ever wondered what it was like to work in a Virtual Command Center? We’re in the background continuously assessing, reviewing and providing interventions to patients at all hours of the day across the nation. Hiring Process -
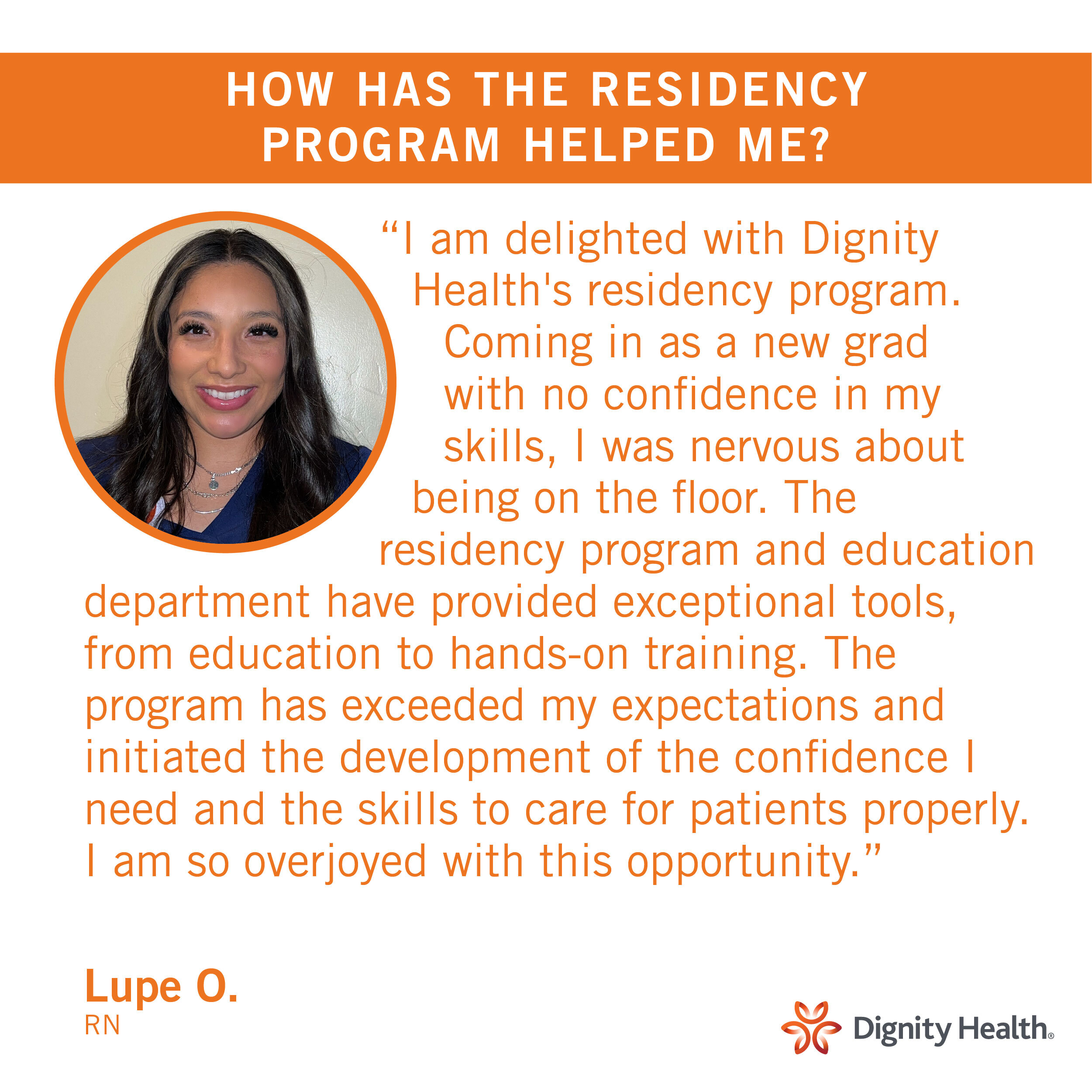
 National Nursing New Grad Residency Program Learn about our new grad nursing program that is nationally-standardized and evidence-based best practice for newly licensed nurses Hiring Process Blog
National Nursing New Grad Residency Program Learn about our new grad nursing program that is nationally-standardized and evidence-based best practice for newly licensed nurses Hiring Process Blog -
 Careers in Environmental Services at CommonSpirit Health Explore career opportunities in Environmental Services at CommonSpirit Health, where we provide a clean and safe environment for patients, staff, and visitors. Hiring Process Blog
Careers in Environmental Services at CommonSpirit Health Explore career opportunities in Environmental Services at CommonSpirit Health, where we provide a clean and safe environment for patients, staff, and visitors. Hiring Process Blog -
 Pursue Your Path as a Medical Assistant at CommonSpirit Health As a Medical Assistant at CommonSpirit Health, you'll be a crucial part of the healthcare system, making a tangible difference in patients' lives. Explore this rewarding career opportunity. Hiring Process Blog
Pursue Your Path as a Medical Assistant at CommonSpirit Health As a Medical Assistant at CommonSpirit Health, you'll be a crucial part of the healthcare system, making a tangible difference in patients' lives. Explore this rewarding career opportunity. Hiring Process Blog -
 CHI Health Career Ladder CNA Program CHI Health has partnered with local Certified Nursing Assistant Programs to offer students C.N.A. training in exchange for full or part-time employment! Hiring Process Blog
CHI Health Career Ladder CNA Program CHI Health has partnered with local Certified Nursing Assistant Programs to offer students C.N.A. training in exchange for full or part-time employment! Hiring Process Blog -
 Meet the CommonSpirit Health Fellows Meet our current CommonSpirit Health Fellows. This is a national, 18-month, system-wide leadership and professional development program that offers a solid foundation for future leaders through hands-on learning experiences, exposure to clinical and non-clinical aspects and mentoring from influential innovators. News/Advancements Blog
Meet the CommonSpirit Health Fellows Meet our current CommonSpirit Health Fellows. This is a national, 18-month, system-wide leadership and professional development program that offers a solid foundation for future leaders through hands-on learning experiences, exposure to clinical and non-clinical aspects and mentoring from influential innovators. News/Advancements Blog -
 On Demand Staffing On Demand Staffing at CommonSpirit Health offers flexible schedules for nurses News/Advancements Blog
On Demand Staffing On Demand Staffing at CommonSpirit Health offers flexible schedules for nurses News/Advancements Blog -
 CommonSpirit Health - NPAC 2025 This is the National Physician Advisor Conference hosted by the American College of Physician Advisors. This conference offers a cross-section of presentations ranging from basic core concepts relevant to any physician advisor to cutting-edge ideas and programs fueling the ongoing transformation of the role. Hiring Process Blog
CommonSpirit Health - NPAC 2025 This is the National Physician Advisor Conference hosted by the American College of Physician Advisors. This conference offers a cross-section of presentations ranging from basic core concepts relevant to any physician advisor to cutting-edge ideas and programs fueling the ongoing transformation of the role. Hiring Process Blog -
 CommonSpirit Health hiring our heroes 12-week Hiring Our Heroes Corporate Fellowship Program. Our first CommonSpirit’s first graduate. Hiring Process Blog
CommonSpirit Health hiring our heroes 12-week Hiring Our Heroes Corporate Fellowship Program. Our first CommonSpirit’s first graduate. Hiring Process Blog -
 CHI Health Locations Now is the perfect time to join our CHI team in one of our locations! Hiring Process Blog
CHI Health Locations Now is the perfect time to join our CHI team in one of our locations! Hiring Process Blog -
 CommonSpirit is Advancing Equitable Opportunities for Hiring and Training CommonSpirit Health is engaged in the Healthcare Anchor Network’s Impact Workforce Commitment, an initiative to hire and train individuals who may have faced employment barriers due to low income, lack of access to education and training, and other socioeconomic challenges. Hiring Process Blog
CommonSpirit is Advancing Equitable Opportunities for Hiring and Training CommonSpirit Health is engaged in the Healthcare Anchor Network’s Impact Workforce Commitment, an initiative to hire and train individuals who may have faced employment barriers due to low income, lack of access to education and training, and other socioeconomic challenges. Hiring Process Blog
Equal Opportunity
CommonSpirit Health™ is an Equal Opportunity/Affirmative Action employer committed to a diverse and inclusive workforce. All qualified applicants will be considered for employment without regard to race, color, religion, sex, sexual orientation, gender identity, national origin, age, disability, marital status, parental status, ancestry, veteran status, genetic information, or any other characteristic protected by law. For more information about your EEO rights as an applicant, please click here [PDF].
CommonSpirit Health™ will not discharge or in any other manner discriminate against employees or applicants because they have inquired about, discussed, or disclosed their pay or the pay of another employee or applicant. However, employees who have access to the compensation information of other employees or applicants as a part of their essential job functions cannot disclose the pay of other employees or applicants to individuals who do not otherwise have access to compensation information, unless the disclosure is (a) in response to a formal complaint or charge, (b) in furtherance of an investigation, proceeding, hearing, or action, including an investigation conducted by the employer, or (c) consistent with the contractor’s legal duty to furnish information. 41 CFR 60-1.35(c). External hires must pass a post-offer, pre-employment background check/drug screen. Qualified applicants with an arrest and/or conviction will be considered for employment in a manner consistent with federal and state laws, as well as applicable local ordinances, ban the box laws, including but not limited to the San Francisco and Los Angeles Fair Chance Ordinances. If you need a reasonable accommodation for any part of the employment process, please contact us by telephone at (415) 438-5575 and let us know the nature of your request. We will only respond to messages left that involve a request for a reasonable accommodation in the application process. We will accommodate the needs of any qualified candidate who requests a reasonable accommodation under the Americans with Disabilities Act (ADA). CommonSpirit Health™ participates in E-Verify.