Provider Relations Specialist
The posted compensation range of $24.59 - $33.81 /hour is a reasonable estimate that extends from the lowest to the highest pay CommonSpirit in good faith believes it might pay for this particular job, based on the circumstances at the time of posting. CommonSpirit may ultimately pay more or less than the posted range as permitted by law.
The purpose of Dignity Health Management Services Organization (Dignity Health MSO) is to build a system-wide integrated physician-centric full-service management service organization structure. We offer a menu of management and business services that will leverage economies of scale across provider types and geographies and will lead the effort in developing Dignity Health’s Medicaid population health care management pathways. Dignity Health MSO is dedicated to providing quality managed care administrative and clinical services to medical groups hospitals health plans and employers with a business objective to excel in coordinating patient care in a manner that supports containing costs while continually improving quality of care and levels of service. Dignity Health MSO accomplishes this by capitalizing on industry-leading technology and integrated administrative systems powered by local human resources that put patient care first.
Dignity Health MSO offers an outstanding Total Rewards package that integrates competitive pay with a state-of-the-art flexible Health & Welfare benefits package. Our cafeteria-style benefit program gives employees the ability to choose the benefits they want from a variety of options including medical dental and vision plans for the employee and their dependents Health Spending Account (HSA) Life Insurance and Long Term Disability. We also offer a 401k retirement plan with a generous employer-match. Other benefits include Paid Time Off and Sick Leave.
One Community. One Mission. One California
Responsibilities
***This position is hybrid.
Position Summary:
The Provider Relations Specialist is responsible for establishing and maintaining positive relationships with various providers across all markets in the Value Hub, building strong, cohesive partnerships. The role is responsible for driving provider engagement and strong communication, supporting network development, managing and improving provider performance, sharing data and insights, and supporting the implementation of quality and care initiatives in partnership with other teams across the Value Hub. Works with internal staff, and other contracted entities to deliver contractual performance standards and ensure customer service objectives are continually met.
Responsibilities may include:
- Develop and maintain effective communication channels with providers, ensuring they are well-informed on key policies, programs, and updates.
- Act as the primary point of contact for providers, addressing their queries, concerns, and feedback promptly and professionally.
- Establish and maintain positive relationships, negotiate favorably, collaborate with others, and build consensus both externally and internally to achieve desired results.
- Mediate conflicts support issues between providers, the Value Hub, and/or health plans ensuring resolutions that align with the network's goals and values
- Conduct ongoing educational training to ensure providers remain compliant and aware of organizational and industry procedures and policies
- Conduct regular site visits to providers' practices to assess their needs and offer tailored support and resources
- Identify and recruit new providers to join the network, in alignment with Value Hub and National strategy, ensuring they meet the network's quality standards and criteria.
- Support provider onboarding and orientation as new providers join the network
- Understand and answer inquiries regarding arrangements contracted with health plans, including plan description, benefit summaries, internal operations workflows, authorizations, and policies & procedures.
- Monitor and evaluate provider performance against established benchmarks and quality metrics, utilize data to identify trends, gaps, and opportunities for network improvement.
- Provide actionable feedback and suggested plans or interventions to support to providers, helping them improve their performance and comply with quality standards.
- Demonstrate ability to understand and interpret laws, rules and regulations as defined under state and Federal statutes along with remaining current on Healthcare Reform updates and changes.
- As applicable, demonstrate familiarity with eligibility, prior authorization, claims administration and provider network administration.
- Understand and interpret regulatory concerns as applicable to new and existing contractual agreements with providers, including HIPAA privacy and security, CMS rules and regulations, and ERISA.
- Communicate effectively with all levels of internal/external staff, management, clients, physicians and physician office staff.
- Create professional documents and presentation using proper grammar, punctuation and appropriate reading level proficient in the use of Microsoft Office applications; Excel, Word, Access, Outlook, PowerPoint, Project.
- Work as part of a team, including other teams within the PHSO and Value Hubs, to ensure continue improvement around network operations and to meet established organizational objectives.
Qualifications
Minimum Qualifications:
- Experience in marketing, sales or customer service in a health care setting required.
- Bachelor’s degree and/or equivalent experience OR 3 or more years' experience working in a similar position in the healthcare industry; or an equivalent combination of training and experience that provide the capabilities needed to perform the job duties. The Provider Relations Representative must have the ability to handle various situations in a professional manner, demonstrating excellent customer service at all times and ability to adapt to change.
- Willingness to work as part of a team, working with others to achieve goals, solve problems, and meet established organizational objectives.
- Strong business acumen, customer service skills, follow-up, organizational and project management skills to ensure objectives and deadlines are consistently met.
- Valid driver’s license and/or reliable transportation required for travel
- Ability to establish and maintain positive business relationships, negotiate favorably, collaborate with others, and build consensus both externally and internally to achieve desired results.
- Demonstrated ability to understand and interpret laws, rules and regulations as defined under state and Federal statutes along with remaining current on Healthcare Reform updates and changes.
- Ability to understand Summary Plan Descriptions, Benefit Summaries, internal operations workflows, and claims policies & procedures.
- Strong problem-solving abilities.
- Ability to identify issues and problems within administrative processes activities, and other relevant areas.
- Familiarity with value-based care health arrangements and programs.
- Ability to understand insights and trends from dashboards and analyzed data outputs to share and recommend practice and operational improvement opportunities to providers.
- Ability to maintain strict confidentiality at all times.
- Ability to continually re-prioritize to meet the needs of internal and external customers throughout the workday.
- Thorough knowledge of generally accepted professional office procedures and processes.
Preferred Qualifications:
- Experience working as an account manager in value-based programs preferred.
Unless directed by a Collective Bargaining Agreement, applications for this position will be considered on a rolling basis. CommonSpirit Health cannot anticipate the date by which a successful candidate may be identified.
Apply
Depending on the position offered, CommonSpirit Health offers a generous benefit package, including but not limited to medical, prescription drug, dental, vision plans, life insurance, paid time off (full-time benefit eligible employees may receive a minimum of 14 paid time off days, including holidays annually), tuition reimbursement, retirement plan benefit(s) including, but not limited to, 401(k), 403(b), and other defined benefits offerings, as may be amended from time to time. For more information, please visit https://www.commonspirit.careers/benefits.
No featured jobs
No recently viewed jobs
You have no saved jobs
-
 Explore Hiring Events at CommonSpirit Health Explore career opportunities at CommonSpirit Health, a leading healthcare organization committed to delivering humankindness. Browse open positions and learn about our mission, values, and benefits.
Explore Hiring Events at CommonSpirit Health Explore career opportunities at CommonSpirit Health, a leading healthcare organization committed to delivering humankindness. Browse open positions and learn about our mission, values, and benefits. -
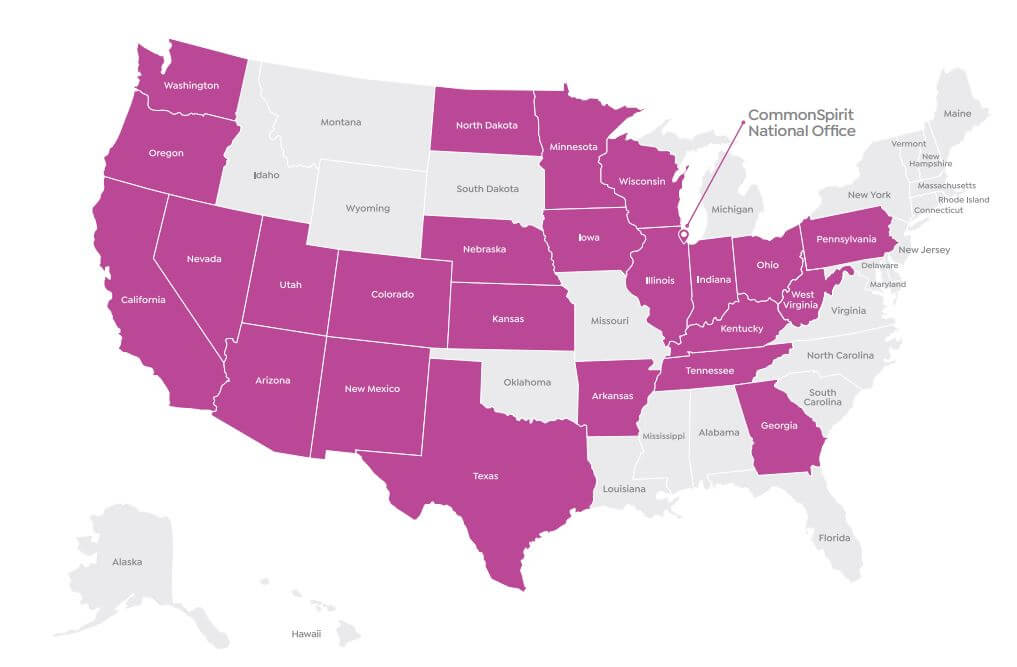
 Our Mission and Vision CommonSpirit was created by the alignment of health care organizations to serve as a single ministry of change.
Our Mission and Vision CommonSpirit was created by the alignment of health care organizations to serve as a single ministry of change. -
 Diversity & Inclusion At CommonSpirit, we are dedicated to delivering humankindness. Diversity is not just an initiative, it’s the true nature of who we are. Related Content
Diversity & Inclusion At CommonSpirit, we are dedicated to delivering humankindness. Diversity is not just an initiative, it’s the true nature of who we are. Related Content -
 About Us Working at Commonspirit
About Us Working at Commonspirit -
 Lead with humankindness - Executive Positions Meaningful work takes a village, but inspired leadership gets it done. At CommonSpirit, our leaders influence by example and succeed through accountability. In character and conduct, you embody humankindness—by pushing us toward our best selves so we can do our best work every day.
Lead with humankindness - Executive Positions Meaningful work takes a village, but inspired leadership gets it done. At CommonSpirit, our leaders influence by example and succeed through accountability. In character and conduct, you embody humankindness—by pushing us toward our best selves so we can do our best work every day. -
 Nursing Explore more about nursing opportunities, our nursing vision and hear from our staff members. Related Content
Nursing Explore more about nursing opportunities, our nursing vision and hear from our staff members. Related Content -
 Our Benefits Our benefits and perks are a big part of why we’re ranked a top employer. Related Content
Our Benefits Our benefits and perks are a big part of why we’re ranked a top employer. Related Content -
 Administrative Fellowship Program The CommonSpirit Health Administrative Fellowship is a national 18-month system-wide fellowship that offers experiential learning and exposure to strategic and operational aspects of an integrated healthcare system.
Administrative Fellowship Program The CommonSpirit Health Administrative Fellowship is a national 18-month system-wide fellowship that offers experiential learning and exposure to strategic and operational aspects of an integrated healthcare system. -
 Recent Graduate Jobs at CommonSpirit Health Earn top-of-class work experience with a nursing leader. As a graduate with the pedigree, tech-savvy, and faith in your own destiny, you embody the next generation of healthcare. At CommonSpirit, our investment in you, personally and professionally, is how we achieve our mission, vision, and values.
Recent Graduate Jobs at CommonSpirit Health Earn top-of-class work experience with a nursing leader. As a graduate with the pedigree, tech-savvy, and faith in your own destiny, you embody the next generation of healthcare. At CommonSpirit, our investment in you, personally and professionally, is how we achieve our mission, vision, and values. -
 Saved Jobs Saved Jobs
Saved Jobs Saved Jobs -
 Legal and Privacy Notices Legal and Privacy Notices
Legal and Privacy Notices Legal and Privacy Notices -
 Terms of Service Terms of Service
Terms of Service Terms of Service -
 Website Privacy Notice Website Privacy Notice
Website Privacy Notice Website Privacy Notice -
 Online Accessibility Notice Online Accessibility Notice
Online Accessibility Notice Online Accessibility Notice -
 Copyrights Copyrights
Copyrights Copyrights -
 Application Notices and Information Learn about CommonSpirit Health's application process, important notices, and requirements. Hiring Process
Application Notices and Information Learn about CommonSpirit Health's application process, important notices, and requirements. Hiring Process -
 CommonSpirit Health Alumni Community Interested in returning to CommonSpirit Health? Learn about jobs, company news, and hear from our employees. Hiring Process Blog
CommonSpirit Health Alumni Community Interested in returning to CommonSpirit Health? Learn about jobs, company news, and hear from our employees. Hiring Process Blog -
 Administrative Fellowship Operations Track The CommonSpirit Health Administrative Fellowship Operations Track will provide fellows with a broad range of health care experiences at the national and local level.
Administrative Fellowship Operations Track The CommonSpirit Health Administrative Fellowship Operations Track will provide fellows with a broad range of health care experiences at the national and local level. -
 Mission Track The CommonSpirit Health Administrative Fellowship Mission Track Fellow will work directly with mission leadership to develop leadership competencies in Mission Integration, Spiritual Care, Community Health, Ethics, and Ministry Formation.
Mission Track The CommonSpirit Health Administrative Fellowship Mission Track Fellow will work directly with mission leadership to develop leadership competencies in Mission Integration, Spiritual Care, Community Health, Ethics, and Ministry Formation. -
 COVID-19 Vaccination Requirements COVID-19 Vaccination Requirements at CommonSpirit Health
COVID-19 Vaccination Requirements COVID-19 Vaccination Requirements at CommonSpirit Health -
 Clinical Engineering Careers at CommonSpirit Health A career in clinical engineering offers a fulfilling blend of technology and healthcare, with the potential to make a positive impact on patient outcomes and the overall efficiency of healthcare delivery. Learn more and explore a career in clinical engineering at CommonSpirit Health. Hiring Process Blog
Clinical Engineering Careers at CommonSpirit Health A career in clinical engineering offers a fulfilling blend of technology and healthcare, with the potential to make a positive impact on patient outcomes and the overall efficiency of healthcare delivery. Learn more and explore a career in clinical engineering at CommonSpirit Health. Hiring Process Blog -
 Learn about our National Travel Nurse Program Join our National Travel Nursing Program and enjoy the variety of a travel nurse with the security of being employed by one of the largest faith-based healthcare systems in the country.
Learn about our National Travel Nurse Program Join our National Travel Nursing Program and enjoy the variety of a travel nurse with the security of being employed by one of the largest faith-based healthcare systems in the country. -
 Learn about our Virtually Integrated Nursing Care Model Virtually Integrated Care provides assistance to the bedside team and patient/family through the use of virtual technology.
Learn about our Virtually Integrated Nursing Care Model Virtually Integrated Care provides assistance to the bedside team and patient/family through the use of virtual technology. -
 Career FAQs Have questions about our hiring process? We're here to assist you if you're ready to apply for a position with CommonSpirit Health.
Career FAQs Have questions about our hiring process? We're here to assist you if you're ready to apply for a position with CommonSpirit Health. -
 Military At CommonSpirit Health, we deeply value the sacrifices made by our veterans and their families. Our commitment to supporting those who served extends beyond words—reflected in the opportunities and benefits we provide. Related Content
Military At CommonSpirit Health, we deeply value the sacrifices made by our veterans and their families. Our commitment to supporting those who served extends beyond words—reflected in the opportunities and benefits we provide. Related Content -
 News & Stories at CommonSpirit Health Visit our News & Stories page and learn more about working at CommonSpirit Health, one of the largest nonprofit health systems in the U.S.
News & Stories at CommonSpirit Health Visit our News & Stories page and learn more about working at CommonSpirit Health, one of the largest nonprofit health systems in the U.S. -
 VMFH Hiring our Heroes VMFH HIring our Heroes
VMFH Hiring our Heroes VMFH HIring our Heroes -
 CHI Health 2025 Nursing Internship CHI Health Nursing Internship in Nebraska Hiring Process Blog
CHI Health 2025 Nursing Internship CHI Health Nursing Internship in Nebraska Hiring Process Blog -
 Upper Midwest Now is the perfect time to join our healthcare team in one of our Upper Midwest locations in Minnesota and North Dakota! Hiring Process Blog
Upper Midwest Now is the perfect time to join our healthcare team in one of our Upper Midwest locations in Minnesota and North Dakota! Hiring Process Blog -
 New Grad Nurse Residency and Transition Program for RNs in California Learn about New Grad Residency and Transition or Fellowship Program for RNs in California Hiring Process Blog
New Grad Nurse Residency and Transition Program for RNs in California Learn about New Grad Residency and Transition or Fellowship Program for RNs in California Hiring Process Blog -
 Innovative Virtual Nursing Model CommonSpirit has two types of virtual nurses: ones who work at a command center to help with admissions, discharges and transfers, and ones who are part of the care team, attending rounds with physicians and being available to patients at the push of the button. Hiring Process Blog
Innovative Virtual Nursing Model CommonSpirit has two types of virtual nurses: ones who work at a command center to help with admissions, discharges and transfers, and ones who are part of the care team, attending rounds with physicians and being available to patients at the push of the button. Hiring Process Blog -
 Radiology Careers at CommonSpirit Health Discover fulfilling career opportunities in Imaging Services at CommonSpirit Health and play a vital role in the diagnosis and treatment of patients' care plans. Hiring Process Blog
Radiology Careers at CommonSpirit Health Discover fulfilling career opportunities in Imaging Services at CommonSpirit Health and play a vital role in the diagnosis and treatment of patients' care plans. Hiring Process Blog -
 Elevate your career as a Surgical Tech with CommonSpirit Health As a surgical technician at CommonSpirit Health, you will play a vital role in guaranteeing that surgical procedures are safe and successful. You will collaborate with leading surgeons and healthcare experts in cutting-edge facilities, providing our patients with the utmost care. Hiring Process Blog
Elevate your career as a Surgical Tech with CommonSpirit Health As a surgical technician at CommonSpirit Health, you will play a vital role in guaranteeing that surgical procedures are safe and successful. You will collaborate with leading surgeons and healthcare experts in cutting-edge facilities, providing our patients with the utmost care. Hiring Process Blog -
 Virtual Command Center Ever wondered what it was like to work in a Virtual Command Center? We’re in the background continuously assessing, reviewing and providing interventions to patients at all hours of the day across the nation. Hiring Process
Virtual Command Center Ever wondered what it was like to work in a Virtual Command Center? We’re in the background continuously assessing, reviewing and providing interventions to patients at all hours of the day across the nation. Hiring Process -
 National Nursing New Grad Residency Program Learn about our new grad nursing program that is nationally-standardized and evidence-based best practice for newly licensed nurses Hiring Process Blog
National Nursing New Grad Residency Program Learn about our new grad nursing program that is nationally-standardized and evidence-based best practice for newly licensed nurses Hiring Process Blog -
 Careers in Environmental Services at CommonSpirit Health Explore career opportunities in Environmental Services at CommonSpirit Health, where we provide a clean and safe environment for patients, staff, and visitors. Hiring Process Blog
Careers in Environmental Services at CommonSpirit Health Explore career opportunities in Environmental Services at CommonSpirit Health, where we provide a clean and safe environment for patients, staff, and visitors. Hiring Process Blog -
 Pursue Your Path as a Medical Assistant at CommonSpirit Health As a Medical Assistant at CommonSpirit Health, you'll be a crucial part of the healthcare system, making a tangible difference in patients' lives. Explore this rewarding career opportunity. Hiring Process Blog
Pursue Your Path as a Medical Assistant at CommonSpirit Health As a Medical Assistant at CommonSpirit Health, you'll be a crucial part of the healthcare system, making a tangible difference in patients' lives. Explore this rewarding career opportunity. Hiring Process Blog -
 CHI Health Career Ladder CNA Program CHI Health has partnered with local Certified Nursing Assistant Programs to offer students C.N.A. training in exchange for full or part-time employment! Hiring Process Blog
CHI Health Career Ladder CNA Program CHI Health has partnered with local Certified Nursing Assistant Programs to offer students C.N.A. training in exchange for full or part-time employment! Hiring Process Blog -
 Meet the CommonSpirit Health Fellows Meet our current CommonSpirit Health Fellows. This is a national, 18-month, system-wide leadership and professional development program that offers a solid foundation for future leaders through hands-on learning experiences, exposure to clinical and non-clinical aspects and mentoring from influential innovators. News/Advancements Blog
Meet the CommonSpirit Health Fellows Meet our current CommonSpirit Health Fellows. This is a national, 18-month, system-wide leadership and professional development program that offers a solid foundation for future leaders through hands-on learning experiences, exposure to clinical and non-clinical aspects and mentoring from influential innovators. News/Advancements Blog -
 On Demand Staffing On Demand Staffing at CommonSpirit Health offers flexible schedules for nurses. News/Advancements Blog
On Demand Staffing On Demand Staffing at CommonSpirit Health offers flexible schedules for nurses. News/Advancements Blog -
 CommonSpirit Health - NPAC 2025 This is the National Physician Advisor Conference hosted by the American College of Physician Advisors. This conference offers a cross-section of presentations ranging from basic core concepts relevant to any physician advisor to cutting-edge ideas and programs fueling the ongoing transformation of the role. Hiring Process Blog
CommonSpirit Health - NPAC 2025 This is the National Physician Advisor Conference hosted by the American College of Physician Advisors. This conference offers a cross-section of presentations ranging from basic core concepts relevant to any physician advisor to cutting-edge ideas and programs fueling the ongoing transformation of the role. Hiring Process Blog -
 CommonSpirit Health hiring our heroes 12-week Hiring Our Heroes Corporate Fellowship Program. Our first CommonSpirit’s first graduate. Hiring Process Blog
CommonSpirit Health hiring our heroes 12-week Hiring Our Heroes Corporate Fellowship Program. Our first CommonSpirit’s first graduate. Hiring Process Blog -
 CHI Health Locations Now is the perfect time to join our CHI team in one of our locations! Hiring Process Blog
CHI Health Locations Now is the perfect time to join our CHI team in one of our locations! Hiring Process Blog -
 CommonSpirit is Advancing Equitable Opportunities for Hiring and Training CommonSpirit Health is engaged in the Healthcare Anchor Network’s Impact Workforce Commitment, an initiative to hire and train individuals who may have faced employment barriers due to low income, lack of access to education and training, and other socioeconomic challenges. Hiring Process Blog
CommonSpirit is Advancing Equitable Opportunities for Hiring and Training CommonSpirit Health is engaged in the Healthcare Anchor Network’s Impact Workforce Commitment, an initiative to hire and train individuals who may have faced employment barriers due to low income, lack of access to education and training, and other socioeconomic challenges. Hiring Process Blog -
 Information Technology The CommonSpirit Health Administrative Fellowship Information Technology (IT) Track will provide fellows with a broad range of experiences in information technology within an integrated health care system.
Information Technology The CommonSpirit Health Administrative Fellowship Information Technology (IT) Track will provide fellows with a broad range of experiences in information technology within an integrated health care system.
Equal Opportunity
CommonSpirit Health™ is an Equal Opportunity/Affirmative Action employer committed to a diverse and inclusive workforce. All qualified applicants will be considered for employment without regard to race, color, religion, sex, sexual orientation, gender identity, national origin, age, disability, marital status, parental status, ancestry, veteran status, genetic information, or any other characteristic protected by law. For more information about your EEO rights as an applicant, please click here [PDF].
CommonSpirit Health™ will not discharge or in any other manner discriminate against employees or applicants because they have inquired about, discussed, or disclosed their pay or the pay of another employee or applicant. However, employees who have access to the compensation information of other employees or applicants as a part of their essential job functions cannot disclose the pay of other employees or applicants to individuals who do not otherwise have access to compensation information, unless the disclosure is (a) in response to a formal complaint or charge, (b) in furtherance of an investigation, proceeding, hearing, or action, including an investigation conducted by the employer, or (c) consistent with the contractor’s legal duty to furnish information. 41 CFR 60-1.35(c). External hires must pass a post-offer, pre-employment background check/drug screen. Qualified applicants with an arrest and/or conviction will be considered for employment in a manner consistent with federal and state laws, as well as applicable local ordinances, ban the box laws, including but not limited to the San Francisco and Los Angeles Fair Chance Ordinances. If you need a reasonable accommodation for any part of the employment process, please contact us by telephone at (415) 438-5575 and let us know the nature of your request. We will only respond to messages left that involve a request for a reasonable accommodation in the application process. We will accommodate the needs of any qualified candidate who requests a reasonable accommodation under the Americans with Disabilities Act (ADA). CommonSpirit Health™ participates in E-Verify.